The Landscape of LGBTQ+ Health Disparities
Much progress has been made in advancing LGBTQ+ health over the last 50 years. As recently as 1974, homosexuality was classified as a mental illness in the DSM (Diagnostic and Statistical Manual of Mental Disorders) — and it was not until 2013 that the manual removed all diagnostic categories based on sexual orientation.
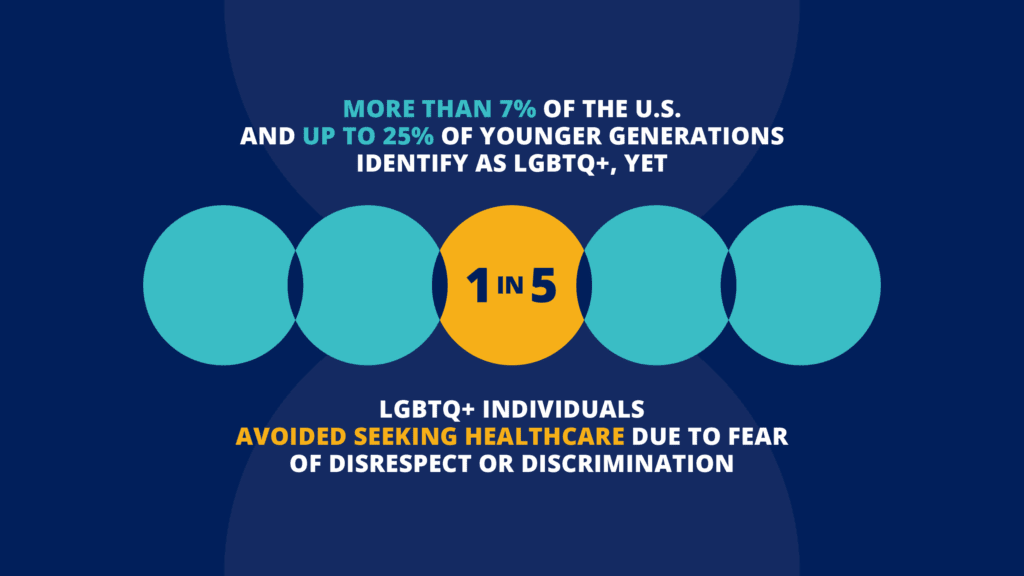
But there is still much work to be done. LGBTQ+ individuals in the United States face significant health disparities rooted in societal stigma and discrimination, poor cultural competency, or an absence of tailored products, services, and programs to address their needs. More than 7% of the U.S. and up to 25% of younger generations identify as LGBTQ+, yet 1 in 5 LGBTQ+ individuals avoided seeking healthcare due to fear of disrespect or discrimination.
By identifying the specific barriers faced by LGBTQ+ individuals, targeted products, services, and programs can be designed to mitigate disparities and promote equal opportunities for advancement. Understanding the unique needs of this population ensures that services are designed to be culturally competent, affirming, and effective, enhancing overall well-being.
Innovations in healthcare delivery, technology development, health research, and policymaking can bridge the existing gaps in the field. In order for these innovations to occur, however, we must ensure that multiple sectors of society are collectively invested in LGBTQ+ health. In other words, we are in dire need of an intersectoral innovation ecosystem committed to address LGBTQ+ health.
Addressing LGBTQ+ health disparities will require structural reforms to our laws and policies, opportunities to advance culturally competent care within healthcare and social services, and greater social engagement across all sectors of society.
Key Health Disparities in LGBTQ+ Communities
Over the years, researchers and advocates have documented well-established disparities across a myriad of health outcomes including mental health, suicidal ideation and behavior, substance misuse, cancer prevention and care, HIV and other sexually-transmitted infections (STIs), cardiovascular diseases, and violence. LGBTQ+ individuals, particularly transgender and gender-nonconforming individuals, also frequently encounter barriers to accessing appropriate and affirming healthcare, leading to delays in necessary services.
The federal public health guidelines, Healthy People 2030, included LGBTQ+ milestones across 7 key areas:
- Bullying among adolescents
- Cancer
- Drug and alcohol use
- Mental health and mental disorders
- HIV/STIs
- Tobacco use
- The inclusion of SOGI data throughout our public health infrastructure.
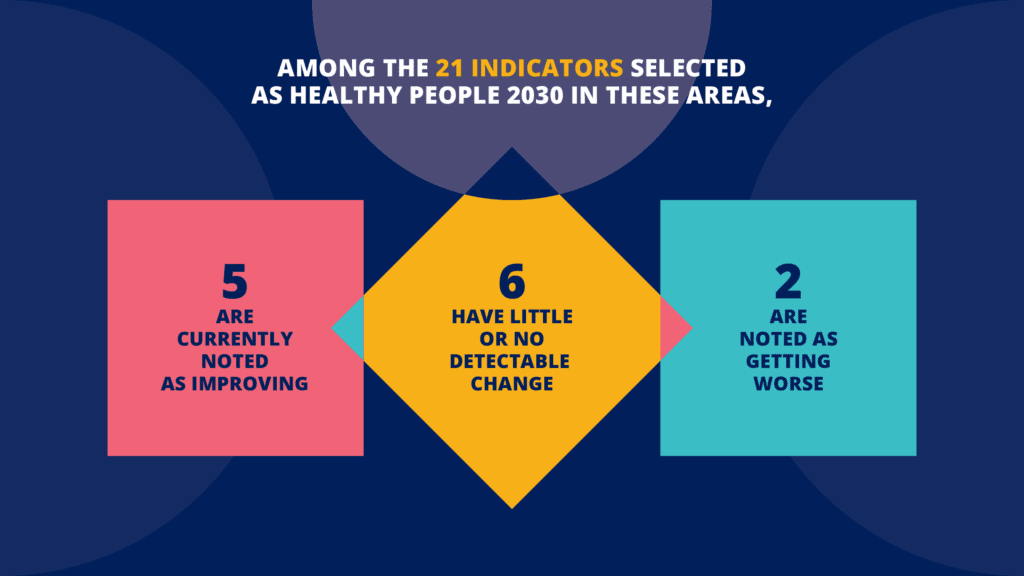
Among the 21 indicators being monitored, interim data from the U.S. Department of Health and Human Services’ Office of Disease Prevention and Health Promotion (OASH) as of February 2025 indicate that five are currently noted as improving, six have little or no detectable change, and two are getting worse. The remaining objectives are noted as only having baseline data to date, or being new objectives for future evaluation and tracking. Of note, none of the trans-specific indicators have progressed.
The Impact of Stigma, Stress, and Trauma on LGBTQ+ Health
LGBTQ+ communities are disproportionately exposed to chronic and compounding forms of stigma, stress, and trauma across their lifespan. These experiences — rooted in societal rejection, discrimination, and violence — undermine quality of life and contribute to excess morbidity and premature mortality. The effects are not confined to mental health alone; they ripple across physical, emotional, and social dimensions of wellbeing, increasing susceptibility to a range of health conditions. To reverse these patterns, programs, products and services must move beyond treating symptoms and instead confront the structural roots of stress and trauma. This includes addressing policy failures, hostile social environments, and persistent underinvestment in LGBTQ+ health.
Structural Conditions Underlying LGBTQ+ Health Disparities
The 2020 report by the National Academies of Sciences, Engineering, and Medicine on LGBTQ+ health disparities emphasized the need to address the broader structural and community-level conditions that shape health outcomes. These include access to quality healthcare, economic stability, educational attainment, family and social support, community and civic engagement, and protective public policies. The report highlights that LGBTQ+ health cannot be disentangled from the systems in which people live, work, and age.
Rather than focusing narrowly on individual behaviors, the report called for comprehensive, systems-level approaches that tackle the root causes of inequality — particularly the role of structural stigma and social exclusion. These upstream factors have cascading effects on both physical and mental health, increasing vulnerability to chronic illnesses such as cardiovascular disease and cancer, while also contributing to elevated rates of depression, anxiety, substance use, and suicidality.
By addressing these structural determinants and investing in environments that foster inclusion, dignity, and safety, we can create the conditions for LGBTQ+ individuals to thrive across the life course. Improving population health outcomes requires transforming the systems that shape daily life — not simply intervening after harm has occurred.
Cultural Competence in the Care of LGBTQ+ Patients
Culturally competent care remains unevenly distributed and largely inaccessible for many LGBTQ+ individuals — especially those living in rural areas or in states with limited legal protections. Geographic location can profoundly shape access to affirming providers, with LGBTQ+ people in underserved or politically hostile regions often facing longer travel distances, fewer provider options, and greater risk of encountering discrimination in care settings.
Even in urban areas with more visible LGBTQ+ communities, culturally competent care is often siloed or scarce. Many health care providers still lack the training, confidence, or institutional backing to understand the lived realities of LGBTQ+ patients, particularly when it comes to intersecting experiences of race, gender identity, immigration status, or disability. This mismatch contributes to medical mistrust, delayed care-seeking, and poor health outcomes.
Expanding culturally competent care requires more than just individual provider training — it necessitates systemic changes in medical education, regulatory frameworks, reimbursement policies, and workforce pipelines. Ensuring that LGBTQ+ people are represented in care design, delivery, and research is essential to mitigating disparities, tailoring services, and building equitable health systems that serve all communities, regardless of zip code.
Social Determinants to Health
The structural deficiencies and cultural norms that lead to LGBTQ+ health disparities and discrimination in healthcare have ripple effects that negatively impact public health at large, yet their impacts are felt most acutely by these marginalized communities. LGBTQ+ individuals are overrepresented in populations experiencing poverty, housing instability, food insecurity, and workplace discrimination. These structural disadvantages are not incidental — they are the result of long-standing exclusion from equitable economic opportunity. The consequences are profound: limited access to stable employment, health insurance, and safe housing restricts access to care and increases vulnerability to illness and injury.
For youth and older adults in particular, the lack of economic safety nets can magnify health risks. LGBTQ+ youth whose families reject them are often cut off from familial financial support, while LGBTQ+ elders frequently face economic hardships after a lifetime of discrimination in employment and benefits systems. For transgender and gender-expansive people, these vulnerabilities are often more severe due to intersecting marginalizations related to gender identity, race, and immigration status.
Time and again, those confronting social hardships and economic insecurity deal with constrained choices and a reduced capacity to seek preventive care, adhere to prescribed medical treatment, or seek timely support. As a result, health disparities are not only more frequent — they are deeper and more enduring. Addressing LGBTQ+ health equity requires that we confront the economic structures that place entire communities at elevated risk and that we build systems of care that account for these social and material realities.
To close the gap, we need more than generalized inclusion: we need strategic, tailored investments across sectors, yet these sectors remain siloed and underleveraged when it comes to addressing the persistent disparities faced by LGBTQ+ communities. On their own, they have neither the infrastructure nor the incentives to generate the systemic change that LGBTQ+ health equity requires.
Eidos Seeks to Change That
Our mission is to build a durable innovation ecosystem where insights and investments across sectors are integrated, not isolated. We serve as a trusted convener—bridging silos between academic researchers, philanthropic funders, community advocates, public sector leaders, and private innovators to foster joint accountability and shared success.
Learn more about the work we do to advance LGBTQ+ health equity.